This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Piriformis Syndrome: How to Manage This Lower-Body Pain Disorder
November 6, 2023

Do you ever experience shooting lower back pains, pain in your hips and buttocks area or a tingling or numbness that extends down to your feet? If so, there’s a chance you have piriformis syndrome.
The good news is there are ways you can help prevent and manage symptoms to get the pain relief you need.
What Is Piriformis Syndrome?
Piriformis syndrome is a type of painful neuromuscular disorder that affects the hips, butt and thighs. It’s caused from spasms in the small piriformis muscle compressing against the sciatic nerve, a thick nerve that runs down the length of the legs.
Sciatica (a common disorder characterized by frequent sciatic nerve pain) and piriformis syndrome are closely related and cause many of the same symptoms, although most cases of sciatic nerve pain are not actually due to piriformis syndrome.
The piriformis muscle, a small muscle located near the hip joint behind the buttocks (the gluteus maximus), has many important functions when it comes to balance, joint stabilization and movement of the lower body. In fact, it’s involved in nearly every function of the hip/buttocks, which is why piriformis syndrome can be really disruptive and aggravating.
Responsible for helping the hip joint lift, rotate and move, the piriformis muscle connects the lower spine to the tops of the thighs and facilitates walking, lifting objects and many other everyday activities we depend on.
The sciatic nerve passes through the piriformis muscle, and the two have many similar roles — so it’s not uncommon for sciatic nerve pain and piriformis syndrome to be confused with one another. The sciatic nerve runs down the back of the leg all the way to the feet, and like the piriformis muscle, it can become overused, leaving you susceptible to numbness, muscle spasms and chronic pain in the surrounding areas.
Once diagnosed, piriformis syndrome is usually treated first with anti-inflammatory and antispasmatic medications. Then, a combination of physical therapy, yoga, stretching and taking time to properly recover from straining movements can all keep the pain away.
Read on for the ways you can manage this painful disorder naturally.
Causes
The underlying cause of piriformis syndrome is entrapment of the sciatic nerve by the piriformis muscle in the buttocks, which can develop on only one side of the body or on both. Many older adults with piriformis syndrome develop physical abnormalities in the muscles around the sciatic nerve, often caused by overuse or past injuries.
There are two types of piriformis syndrome: primary (caused by a anatomic change, such as a split muscle or nerve) and secondary (caused by any precipitating cause, including trauma). Research shows that secondary cases are much more common — among patients with piriformis syndrome, fewer than 15 percent of cases have primary causes.
It’s estimated that at least 6 percent, and as may as 36 percent, of those who have been diagnosed with back pain disorders actually have piriformis syndrome. People develop piriformis syndrome for different reasons — sometimes due to straining/overworking the muscles near the hips or butt during work or exercise, experiencing trauma or an injury to the lower body, or developing high amounts of bodywide inflammation that aggravates weak/strained muscles.
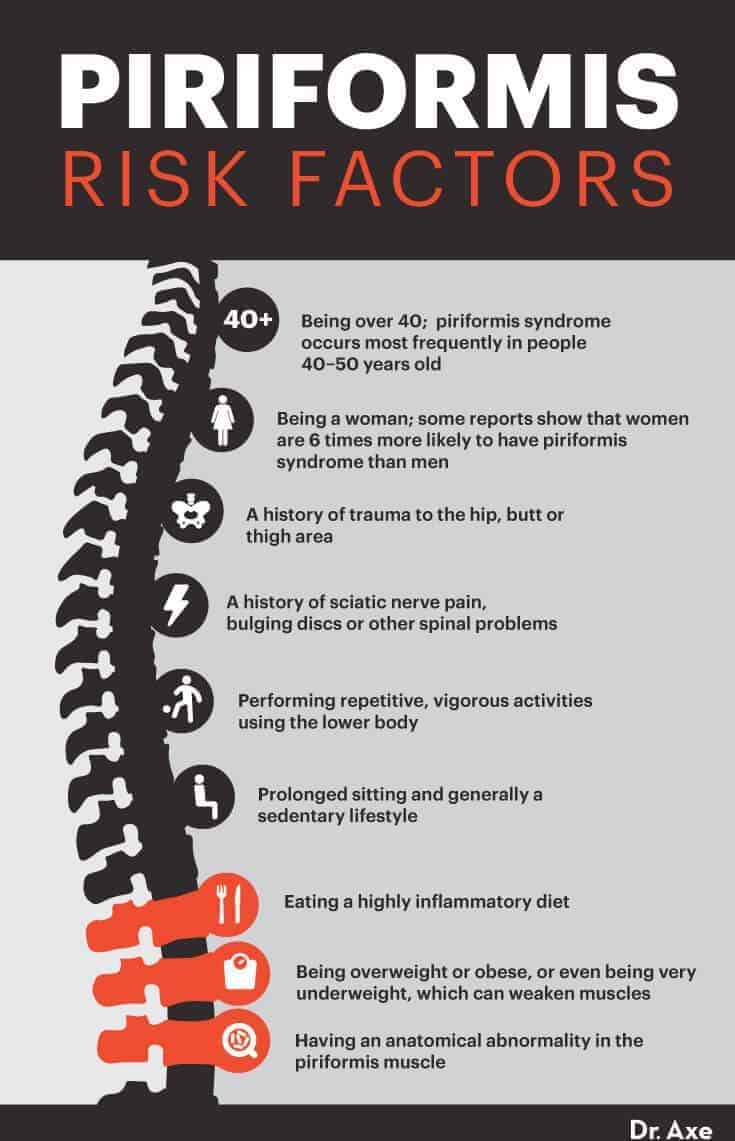
Risk factors for piriformis syndrome include:
- being over the age of 40; piriformis syndrome occurs most frequently in people 40–50 years old
- being a woman; researchers believe more woman are affected than man due to biomechanics associated with the wider quadriceps/hips of women’s bodies — some reports show that women are six times more likely to have piriformis syndrome than men
- a history of trauma to the hip, butt or thigh area
- having a history of sciatic nerve pain, bulging disc or other spinal problems
- performing repetitive, vigorous activities using the lower body (especially long-distance running, squatting and walking using improper form, without enough rest in between training)
- prolonged sitting — either at your desk at work or during a commute in the car, for example — which can lead to forward head posture and a sedentary lifestyle
- eating a highly inflammatory diet, which raises risk for deficiencies and electrolyte imbalance
- being overweight or obese, or even being very underweight, which can weaken muscles
- having an anatomical abnormality in the piriformis muscle (a less common cause)
Symptoms
Symptoms of piriformis syndrome range in terms of intensity. Sometimes ongoing muscle aches and pains are experienced nearly every day and make it hard to go about life normally. Other times this condition comes and goes and is pretty mild.
Many people experience progressive worsening of symptoms over several months as the piriformis muscle becomes more inflamed and irritated, especially if reoccurring movements that aren’t stopped are the underlying cause of the pain.
The most common symptoms of piriformis syndrome include:
- Pain near the hips and butt
- tingling or numbness in the lower body, including the feet
- shooting lower back pains that extend down the length of the leg through the sciatic nerve (this condition is called sciatica), which can disturb sleep and make it hard to move normally
- pain when standing or sitting for long periods of time
- trouble walking, lifting objects, bending over, climbing stairs or exercising
- sometimes backaches, neck pains and headaches
- abdominal pain and trouble going to the bathroom
Diagnosis
Piriformis syndrome is notoriously misdiagnosed and often hard for doctors to spot, commonly confused with sciatic nerve pain, herniated discs and other problems. It’s important to get a proper diagnoses so you can target the underlying issue and stop repetitive movements that might make the problem worse.
Doctors use a combination of a physical exam, taking a patient’s medical history and stretching/applying pressure to the piriformis muscle to test for pain in order to make a diagnosis of piriformis syndrome. As of now, there is no definitive test for piriformis syndrome (it’s not detectable using X-rays, for example), which means assessing the patient’s pain and symptoms is the best way to make a diagnosis and start treatment.
However, MRIs are also sometimes used to rule out other similar conditions, like compression of the sciatic nerve from a herniated or bulging disc in the back or an infection.
Many doctors position patients in certain ways to test for pain in the piriformis muscle. Having the patient lay down on his or her side, internally rotating the top leg and crossing the top foot over the bottom foot extends the alpha angle of the piriformis muscle, which should cause noticeable pain if the patient is in fact suffering from piriformis syndrome. FAIR (flexion, adduction and internal rotation testing) tests are is done using this method to test sciatic symptoms by stabilizing the hip, then internally rotating and adducting the hip while applying downward pressure to the knee.
Treatment
Effective treatment for piriformis syndrome depends on what’s causing the underlying muscular damage to begin with, so seeing a professional for a proper diagnoses and advice is the first step in resolving symptoms. After a diagnoses is made, many doctors recommend short-term steroid or anaesthetic injections for stopping muscle spasms and lowering inflammation and pain around the nerves near the piriformis muscle. Your doctor might also possibly prescribe other medications, like anti-inflammatory drugs or muscle relaxers.
Injections or medications can be helpful for resolving symptoms quickly and starting you on a path to recovery — however, they aren’t a long-term solution. Ongoing relief from piriformis syndrome usually requires making lifestyle changes, including changing your exercise routine, eating a healthy diet, adjusting your posture and form, and possibly seeing a physical therapist or chiropractor for chiropractic adjustments.
Here are ways to treat and manage symptoms:
1. Physical Therapy and Osteopathic Adjustments
Many doctors feel that physical therapy and osteopathic adjustments performed by a doctor are two of the best ways to resolve piriformis pain, since these can effectively address underlying problems, such as poor form/posture during exercise or sciatic nerve pain that contributes to inflammation and pain around the piriformis muscle.
A physical therapy protocol for treating piriformis syndrome can include stretching, strengthening and mobilizing the hip joints in various ways, using specific exercises that flex and loosen the appropriate areas. Your therapist might perform myofascial release using a foam roller along the hip thighs and buttocks to break up tissue adhesions and improve healing.
Hip joint mobilization; hamstring stretches; and strengthening the quadriceps, lower back and core are all important for preventing future symptoms from returning.
When visiting an osteopathic physician, osteopathic manipulative treatments can be performed to restore normal range of motion of the hip and decrease pain. Two common exercises are called counterstrain and facilitated positional release, which remove tension from the piriformis muscle.
The patient lies in a prone position with the affected side of the body at the edge of the examination table while the osteopathic physician carefully brings the patient’s affected leg over the side of the table, placing it into flexion at the hip and knee, with abduction and external rotation at the hip. This is held for anywhere between 1.5–5 minutes.
2. Yoga and Stretching
Certain stretches or yoga poses can help strengthen the core, lower back, hips and quads/buttocks while also loosening up and supporting the piriformis muscle. In particular, the strengthening of the adductor muscles of the hip has been shown to be beneficial for patients with piriformis syndrome.
You can practice targeted exercises or stretches at home on your own, but it’s a good idea to be taught by a professional first to make sure you don’t injure yourself even more.
Over the long term, lengthening the legs and spine through yoga or other exercises can also help develop good posture, which reduces stiffness, inflammation and pain along the sciatic nerve. Studies have found that yoga is safe and effective for people with piriformis syndrome and sciatic nerve pain.
Some of the most important movements for preventing sciatic pain target the hips, hamstrings, glutes and lower back, while building strength in the core and legs and relaxing stiff areas.
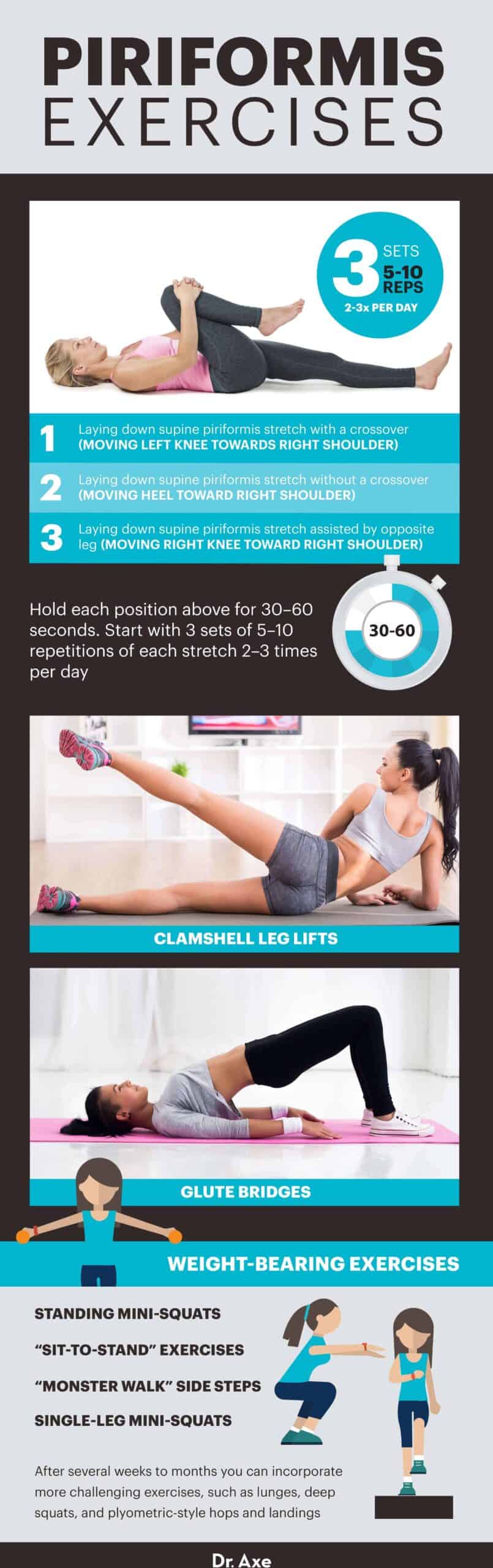
The following piriformis exercises can be helpful to do several times per week or more:
- Laying down supine piriformis stretch with a crossover (moving left knee toward right shoulder).
- Laying down supine piriformis stretch without a crossover (moving heel toward right shoulder).
- Laying down supine piriformis stretch assisted by opposite leg (moving right knee toward right shoulder).
- Hold each position above for 30–60 seconds, and start with three sets of five to 10 repetitions of each stretch two or three times per day.
- After you’ve built up tolerance and pain reduces, you can start to add more weight to hips. At this point you can strengthen legs and hips by performing glute bridges and clamshell leg lifts or weight-bearing exercises, such as standing mini-squats, “monster walk” side steps, “sit-to-stand” exercises and single-leg mini-squats.
- After several weeks to months, you can incorporate more challenging exercises, such as lunges, deep squats, and plyometric-style hops and landings.
3. Rest and Recover the Right Way
Taking a break from repetitive movements or exercises can give the piriformis muscle time to heal, which is important for proper muscle recovery. Try beginning by reducing the types of aggravating exercises/movements you do daily, especially those that put pressure on the hips.
Movements and postures that tend to make pain worse include driving or sitting at a desk for a long period, long-distance running, walking/running up hills, squatting, playing tennis, shortening the spine by bringing the knees toward the chests, or climbing stairs.
Most treatment plans call for more movement in general to improve strength and mobility (meaning less sitting for prolonged periods) along with targeted exercises to loosen up inflamed areas. Make sure to always stretch and warm up properly when exercising to avoid injuries.
You can practice certain stretches and exercises at home without the need for a doctor visit once you have the hang of them. You can also try to alternate periods of sitting/lying down with short walks during the day to stay active, but allow for more rest between exercises if needed.
4. An Anti-Inflammatory Diet and Supplements
Certain lifestyle, personal and occupational risk factors make it more likely that someone will suffer from muscle and nerve pains. These include older age, high levels of mental stress that tenses muscles, being overweight or obese, sitting for long periods, cigarette smoking, and eating a low-nutrient diet. All of these can increase inflammation, which makes it harder to heal from injuries and increases pain, swelling and complications.
Eating a nutrient-dense, low-processed diet and taking supplements might be able to help you heal faster, maintain a healthy weight over time, and recover better from exercise or training. Try lowering your intake of things like sugar, processed meats, chemically sprayed crops, refined grain products, alcohol and packaged snacks.
Include more high-potassium foods and sources of magnesium, including leaf green veggies, sweet potatoes and avocados, to lower muscle spasms and pain. Healthy fats, such as extra virgin olive oil and coconut oil, are also important, along with “clean and lean proteins” (cage-free eggs, grass-fed meat, wild-caught fish) and fermented foods and other probiotic foods.
Other important factors for reducing bodywide inflammation include avoiding smoking/recreational drugs, lowering stress and sleeping well. Additionally supplements that can help include omega-3 supplements, magnesium, turmeric and CoQ10.
5. Managing Pain
Certain studies have found that many patients benefit from using cold and heating packs to lower pain naturally, which relax muscles almost immediately and can prevent more inflammation. These seem to work especially well if performed before physical therapy or stretching sessions at home because they can lower muscle discomfort associated with direct treatment applied to an irritated or tense piriformis muscle.
If you injured yourself due to trauma, avoid heat right away. However, after a few days try using inexpensive heating pads set on a low or medium setting, placed on the hips while laying down for about 15 to 20 minutes every day.
Another similar approach that works well is taking warm bathes, especially if you add a muscle-soothing essential oil like peppermint oil, which naturally relaxes muscle spams. Heat loosens up tight muscles and helps increase circulation, but as an alternative to heat, applying an ice pack for 10 to 15 minutes every two to three hours does the trick too.
Acupuncture and professional massages might also be able to help you manage pain. Acupuncture, which uses tiny needles to target specific pathways in the body, has been approved by the U.S. Food and Drug Administration as a treatment for chronic pain and is supported by various studies in relation to reducing chronic muscle pains (including sciatica and piriformis syndrome).
Similarly, massage therapy is another nonsurgical, holistic approach to managing muscular pains, since it helps improve blood flow, breaks up tissue adhesions and even releases endorphins, which act like natural pain relievers.
Conclusion
- Piriformis syndrome is a type of painful neuromuscular disorder that affects the hips, butt and thighs. It’s caused from spasms in the small piriformis muscle compressing against the sciatic nerve, a thick nerve that runs down the length of the legs. Sciatica (a common disorder characterized by frequent sciatic nerve pain) and piriformis syndrome are closely related and cause many of the same symptoms, although most cases of sciatic nerve pain are not actually due to piriformis syndrome.
- The most common symptoms of piriformis syndrome include pain near the hips and butt; tingling or numbness in the lower body; shooting lower-back pains that extend down the length of the leg through the sciatic nerve; pain when standing or sitting for long periods of time; trouble walking, lifting objects, bending over, climbing stairs or exercising; backaches, neck pains and headaches; and abdominal pain and trouble going to the bathroom.
- People develop piriformis syndrome for different reasons — sometimes due to straining/overworking the muscles near the hips or butt during work or exercise, experiencing trauma or an injury to the lower body, or developing high amounts of bodywide inflammation that aggravates weak/strained muscles.
- Ongoing relief from piriformis syndrome usually requires making lifestyle changes, including changing your exercise routine, eating a healthy diet, adjusting your posture and form, and possibly seeing a physical therapist or chiropractor for adjustments.
